Understanding the Hysterectomy Risk of Death: A Comprehensive Guide for Patients and Practitioners
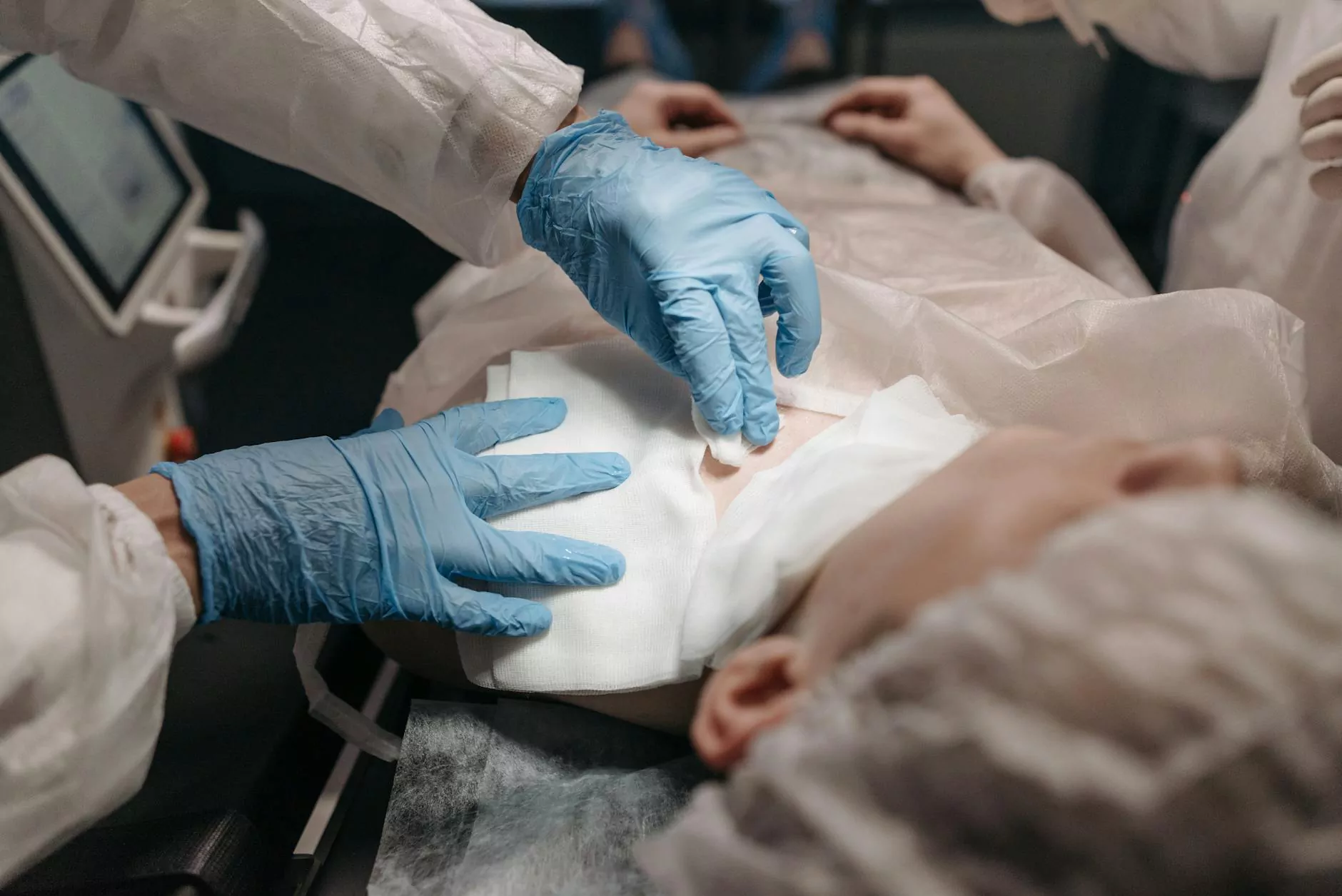
When considering a hysterectomy, one of the most critical concerns that often arises is the hysterectomy risk of death. While modern surgical techniques and medical advancements have significantly improved the safety profile of this common procedure, understanding the potential risks, including rare but serious complications, remains vital for both patients and healthcare providers. This detailed guide aims to offer thorough insights into what influences the hysterectomy risk of death, how it can be minimized, and why consulting highly qualified Obstetricians & Gynecologists is crucial for ensuring a safe surgical journey.
What Is a Hysterectomy and Why Is It Performed?
A hysterectomy is a surgical operation to remove the uterus. It can be performed for multiple reasons, including:
- Uterine fibroids causing severe symptoms
- Chronic uterine bleeding unresponsive to other treatments
- Endometriosis
- Uterine prolapse
- Uterine cancer or precancerous conditions
- Adenomyosis
- Chronic pelvic pain
The procedure's approach varies from total hysterectomy (removal of the uterus and cervix) to partial or subtotal hysterectomy (removing only the uterus body), with options like laparoscopic, abdominal, or vaginal methods, depending on the patient's condition and surgeon’s expertise.
Understanding the Hysterectomy Risk of Death
The hysterectomy risk of death is a vital consideration that has decreased markedly over the decades. Due to advancements in surgical technology, anesthesia, and infection control, the mortality rate associated with hysterectomy today remains very low. However, it is not zero, and several factors can influence the overall risk profile.
Statistical Perspective on the Hysterectomy Risk of Death
Contemporary studies indicate that the risk of death from hysterectomy is approximately 0.1% to 0.2%. This means out of 1,000 women undergoing the procedure, roughly 1 to 2 women might face complications that could lead to mortality. These statistics emphasize the importance of selecting experienced surgical teams and comprehensive preoperative evaluations.
Major Factors Impacting the Hysterectomy Risk of Death
Several influential elements determine the likelihood of mortality during or after a hysterectomy:
- Patient’s Overall Health: Chronic conditions like heart disease, diabetes, respiratory issues, or obesity increase surgical risks.
- Type of Hysterectomy: More complex or emergency procedures generally carry higher risk profiles.
- Surgical Approach: Minimally invasive techniques such as laparoscopic or vaginal hysterectomy tend to have lower complication rates compared to open abdominal surgery.
- Age: Older women often face increased risk due to comorbidities.
- surgeon’s Experience and Facility Resources: Experienced surgeons with access to well-equipped hospitals significantly reduce risks.
- Preoperative Preparation: Proper patient assessment and management of existing conditions are vital.
Risk Factors Associated with Increased Hysterectomy Mortality
Recognizing factors that elevate the hysterectomy risk of death helps clinicians and patients make informed decisions. These include:
- Advanced Age: Higher age often correlates with increased perioperative risk due to decreased physiological reserve.
- Severe Medical Comorbidities: Conditions like cardiovascular disease, uncontrolled hypertension, or severe respiratory illnesses amplify perioperative dangers.
- Emergency Surgeries: Surgeries performed under urgent conditions tend to have higher complication rates.
- Infection or Sepsis: Pre-existing infections can complicate recovery and raise mortality risk.
- Heavy Bleeding or Hemorrhage: Significant intraoperative bleeding can lead to shock if not managed promptly.
How Can the Hysterectomy Risk of Death Be Minimized?
Understanding and implementing safety measures significantly reduce the hysterectomy risk of death. Key strategies include:
- Thorough Preoperative Evaluation: Comprehensive health assessments and optimization of existing conditions.
- Choosing the Right Surgical Approach: Minimally invasive procedures like laparoscopic or vaginal hysterectomy are generally safer for suitable candidates.
- High-Quality Surgical Care: Conducting the procedure in accredited hospitals by experienced obstetricians & gynecologists.
- Utilization of Advanced Surgical Technology: Use of robotic surgery or enhanced visualization tools improves precision and safety.
- Perioperative Monitoring: Continuous patient monitoring and readiness for managing hemorrhage or complications.
- Postoperative Care: Close observation for signs of infection, bleeding, or other complications.
The Role of Experienced Obstetricians & Gynecologists in Reducing Hysterectomy Risk of Death
The expertise and specialization of Obstetricians & Gynecologists play a pivotal role in ensuring the safety of hysterectomy procedures. These specialists possess advanced training to handle complex cases, anticipate potential complications, and manage emergencies with utmost professionalism.
When considering a hysterectomy, consult a doctor from reputable institutions, such as drseckin.com. Their team of expert physicians emphasizes personalized care, meticulous planning, and adherence to the highest safety standards, all of which contribute to lowering the hysterectomy risk of death.
Postoperative Prognosis and Long-term Outcomes
Thanks to advances in surgical techniques and postoperative management, women undergoing hysterectomy today generally experience excellent outcomes with low mortality rates. The focus is not only on survival but also on improving quality of life by alleviating debilitating symptoms caused by benign or malignant gynecological conditions.
Patients should maintain regular follow-up visits, adhere to postoperative instructions, and consult their doctors promptly if any unusual symptoms arise.
Conclusion: Prioritizing Safety to Minimize the Hysterectomy Risk of Death
While the hysterectomy risk of death is statistically very low, it remains a significant consideration that underscores the importance of choosing qualified healthcare providers, comprehensive pre-surgical planning, and appropriate surgical techniques. Patients insured with highly skilled obstetricians & gynecologists, like those at drseckin.com, benefit from safer surgical outcomes and peace of mind.
Ultimately, informed decision-making, coupled with expert care, ensures that hysterectomy remains a safe and effective treatment option for women facing complex gynecological issues. The minimal hysterectomy risk of death today signifies the remarkable progress in medical science—yet, continued vigilance and personalized care are critical for sustaining these safety standards.









